Did you know that osteoporosis affects 54 million adults over the age of 50 every year? Or, that these numbers will rise to 64.4 million by 2030?
Much emphasis has been placed on women suffering from the disease. But, in truth, osteoporosis knows no gender boundaries.
In fact, by the age of 65 to 70, both genders experience bone loss at the same rates. Older men and women also prove less capable of absorbing calcium, an essential mineral crucial to healthy bone development.
So, how do you maintain optimal bone health as you age? Let’s take a look at the role that testosterone plays in bone building and health.
What Is Osteoporosis?
Literally “porous bone,” osteoporosis is a disease that affects the quality and density of bone. As bones become more fragile and porous, the risk for fractures rises.
You may have heard of osteoporosis referred to as a “silent disease.” This proves an apt and accurate description as the disease goes largely undiagnosed until a fracture occurs. In essence, a break represents your first symptom.
Our bones are living tissue. They fluctuate throughout our lives. From infancy to our 30s, these changes result in increased bone development and strengthening.
But once we reach peak bone mass, the bone matrix may dissolve. When it does so more quickly than it can be replaced, this leads to osteopenia and then osteoporosis.
For those suffering from osteoporosis, bones become increasingly brittle and riddled with weakness. Hip fractures prove the most dramatic symptom of osteoporosis. But other common fractures include those of the wrist and spine.
Spinal fractures can lead to a loss of height, They can also result in intense back pain and deformities of the spine such as Dowager’s Hump.
Osteoporosis 101
It may not surprise you to hear that one in three women in the world suffers from this condition. But did you know that one in five men over the age fifty also suffer from osteoporosis?
Doctors tend to focus on the risks of osteoporosis more in postmenopausal women than aging men. So, you might not be aware you’re even at risk.
Why does most of the osteoporosis attention go to women? Because women tend to see a steep drop off in bone density following menopause.
Women also have smaller skeletons to begin with. This means any loss proves proportionally more devastating. But just because men have bigger skeletons and don’t go through menopause, doesn’t mean they’re immune.
Osteoporosis is a debilitating disease. It results from aging, and cases will continue to skyrocket as life expectancy increases.
Men are often much older when they get diagnosed with osteoporosis. This often comes as the result of a hip fracture.
As a result of their increased age and the severity of their fractures, men prove more likely to die from osteoporosis-related complications than women.
The Types of Osteoporosis
Did you know that there are actually two types of osteoporosis? They are known as primary and secondary osteoporosis.
Primary osteoporosis refers to age-related bone loss. You may see it referred to as senile osteoporosis.
Idiopathic osteoporosis is a term used specifically for men under the age of 70 who experience bone mass loss. These younger men are usually diagnosed with secondary osteoporosis. This basically means that a secondary factor (other than age) is causing the loss.
Factors Leading to Osteoporosis in Men
What types of factors can increase bone loss in younger men? These include certain lifestyle behaviors, diseases, and medications.
More specifically, causes of osteoporosis in men include:
- Hypogonadism (low testosterone levels)
- Smoking
- Excessive drinking
- Systemic mastocytosis
- Neoplastic disease
- Homocystinuria
- Ankylosing spondylitis
- Rheumatoid arthritis
- Osteogenesis imperfecta
- Hyperparathyroidism
- Hypercalciuria
- Thyrotoxicosis
- Immobilization
- Chronic obstructive pulmonary disease
- Asthma
- Gastrointestinal disease
- Cystic fibrosis
- Immunosuppressive drugs
- Glucocorticoid medications
The trends underlying these diagnoses include chronic diseases that affect the lungs, kidneys, stomach, and intestines.
Chronic diseases and conditions that affect hormone levels, such as testosterone, also play a huge role in the weakening of the body’s bone structure.
Undiagnosed hormonal issues, particularly low T, also impact bone health among older men. White males appear to be at a much higher risk, and with each passing birthday, your likelihood of developing osteoporosis skyrockets.
Unhealthy lifestyles and regular use of certain medications also up your chances of developing fractures.
Many causes of osteoporosis in men arise as secondary to low testosterone levels. After all, certain medications and gastrointestinal conditions, such as celiac disease, lead to decreased testosterone production. And this results in bone mass loss.
Fortunately, testosterone replacement therapy represents a missing piece of the puzzle for many men suffering from a compromised bone structure.
Your Body’s Hormone Center
When we talk hormones, we’re referring to the body’s endocrine system. The endocrine system represents a complicated collection of glands. These glands rely on direction from the brain to keep hormone levels consistent and healthy.
The endocrine system controls a wide variety of bodily functions including:
- Growth and development
- Metabolism
- Tissue function
- Reproduction
- Sexual function
- Sleep
- Mood
Besides the glands of the human body, the endocrine system also involves the pancreas and the testicles in males.
Testosterone remains essential to the development of strength and muscle bulk. It also increases the amount of growth hormone present in an individual, which, in turn, leads to increased levels of growth hormone.
Higher growth hormone levels ensure that exercise leads to muscle building. Testosterone plays a role in the metabolism of fat, so when your levels run low, you may gain weight.
Testosterone also affects bone density. How? The hormone tells bone marrow to create more red blood cells.
Hypogonadism or Low Testosterone Levels
Decreasing estrogen levels, like those experienced by women during menopause, remain the infamous culprit in osteoporosis in women. Now researchers believe lowered sex hormone levels in men can lead to the same condition.
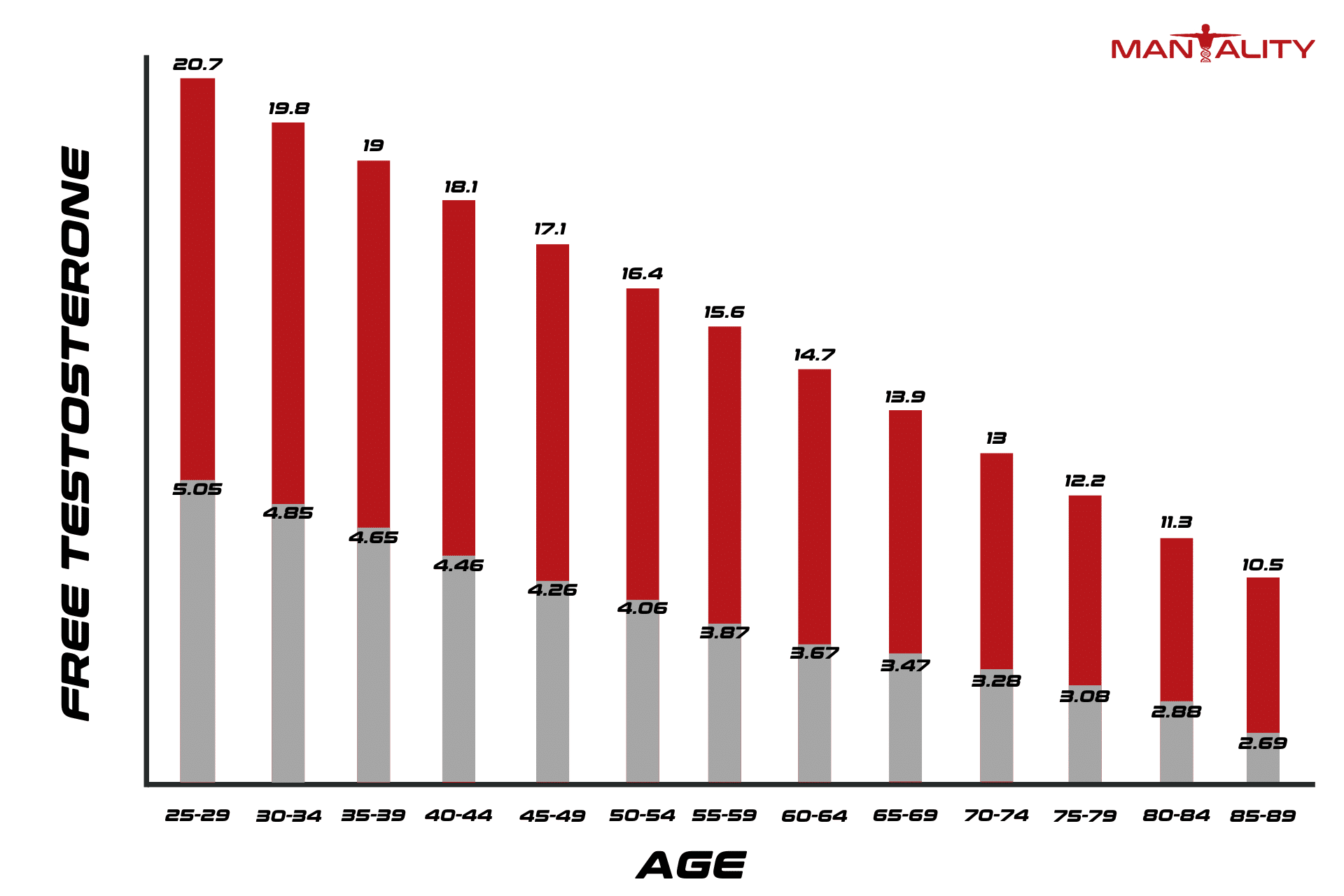
Testosterone remains the essential male hormone. Male infants begin producing testosterone within seven weeks of conception. These levels will fluctuate throughout a man’s lifetime with a peak in levels during the late teenage years.
By the age of 30, it’s normal to start seeing testosterone levels decrease. But this should be a gradual decrease. Not a sudden drop-off.
When a sudden drop occurs, it mimics the effects of menopause on women. What does this mean for men? A faster and potentially debilitating loss of bone mass.
Lack of testosterone in men is known as hypogonadism. Hypogonadism should be closely monitored. It can and should be treated with hormone replacement therapy.
Not only will this therapy help safeguard bones, but it helps in other areas (such as your sex life), too.
Links Between Low Testosterone and Bone Mass Loss
But how strong are the linkages between lower testosterone levels and bone loss? One study of 235 hypogonadal men aged on average 51 years found that 39 percent had osteopenia. Another five percent had full on osteoporosis.
Osteopenia refers to the midway point between bone health and osteoporosis. This condition (when left untreated) is likely to degrade into osteoporosis.
In other words, osteopenia is a condition where your body gets rid of more bone tissue than it replaces.
This is one of several groundbreaking studies that have demonstrated clear links between low testosterone and bone loss in men.
Fortunately, testosterone replacement therapies offer a readily available and effective treatment for osteoporosis in men. This therapy should be coupled with a healthy diet and a regular exercise regimen for optimal results.
Monitoring Your Testosterone Levels
This begs the question: how do you know if testosterone replacement therapy is right for you?
Studies show that between two and six million men in the US alone suffer from hypogonadism. Yet, it remains one of the most under-diagnosed conditions. Of those affected, only about five percent receive the treatment that they need.
If you are experiencing symptoms such as weight gain, erectile dysfunction or reduced sex drive, then you may be a candidate for hormone replacement therapy.
Since testosterone travels through your circulatory system, a blood test can help your doctor determine whether or not you suffer from hypogonadism.
Because low testosterone and osteoporosis are interconnected, diagnosing hypogonadism could also represent a form of early detection for osteoporosis. Before a fracture changes your life forever.
Because testosterone levels fluctuate throughout the day, however, you may need to submit to more than a blood test. Or, your health practitioner may opt for a blood test first thing in the morning when testosterone levels prove highest.
Once your physician has determined whether or not you suffer from low testosterone levels, you can move forward with hormone replacement therapy.
Hormone Replacement Therapy for Low T
Once you’ve been diagnosed with low levels of testosterone in your system, your doctor will prescribe you with a hormone replacement therapy. For many men, this proves as simple as a gel or cream that you rub on your arms and shoulders.
However, you must be careful not to transmit any of the cream or gel to others through skin-on-skin contact.
For some, a better therapy proves an intramuscular shot administered by your physician. There’s also a patch that can be placed on the skin. The patch slowly administers testosterone into your circulatory system via your skin.
Some patients even opt for pellets that are placed directly under the skin or oral replacement therapies. Contact your doctor to learn more about the replacement treatments that are available and which one’s right for you.
Remain Committed to an Osteoporosis Treatment Plan
Diagnosing male osteoporosis may involve a full medical workup. During this consultation, be prepared to provide a full medical history as well as blood and urine samples.
Your doctor will also take x-rays of your skeletal structure for evaluation as well as order a bone mineral density (BMD) test. A BMD test indicates your current fracture risk.
The most common type of BMD proves painless and similar to an x-ray. But it results in far less exposure to radiation. Called a central dual-energy x-ray absorptiometry or central DXA test, it measures bone density at the spine and hip.
X-rays and the BMD test will also provide a baseline to analyze how well your bones respond to osteoporosis treatment.
No matter what your doctor recommends, remember to commit fully to treatment. That means going in for regular bone density screenings to see how testosterone therapy is impacting your overall bone density scores.
To optimize bone health and minimize loss, your physician may also ask you to take additional medications to prevent osteoporosis.
Commit to a Healthy Lifestyle
Besides exploring testosterone replacement therapy with your doctor, you should also consider implementing a healthy lifestyle. Avoid smoking and excess alcohol consumption.
What’s more, eat for healthy bones. That means lots of leafy greens and vegetables as well as calcium and vitamin D supplements to ensure optimal daily intakes for your age.
Increasing your daily physical activity levels also proves important. Focus on weight-bearing exercises such as:
- Jogging
- Racquet sports
- Climbing stairs
- Walking
- Team sports
These activities should force your muscles to work against gravity.
That said, consult with your doctor about exercise regimens that involve lots of twisting such as golf, basketball, and tennis if you’ve already been diagnosed with osteoporosis. You may need to curtail these sports to stay fracture free.
Bone Health and Testosterone Levels
When it comes to bone health, recognizing low testosterone as a factor in osteoporosis could help you prevent injuries down the road. What’s more, if you already demonstrate the signs of low T, time is of the essence.
Fortunately, once diagnosed with hypogonadism, osteopenia, or even osteoporosis, you can reverse these conditions by working with a skilled practitioner who understands the relationship between low T and bone density.
After running a variety of medical tests to confirm the condition and create a baseline for your treatment moving forward, you’ll be able to start reaping the benefits of testosterone replacement therapy.
These include increased muscle mass, increased metabolism, and increased sexual drive. Ready for more info about testosterone? Learn more about its relationship to zinc and your health.